Best Revenue Cycle Management Software of 2026 and Why They’re Worth Knowing
As an organization, we recognize the importance of sustaining consistent revenue performance and the pivotal role that Revenue Cycle Management (RCM) software plays in achieving financial stability. With healthcare reimbursement models growing increasingly complex, selecting the right RCM solution has become a strategic imperative rather than an operational afterthought.
While exploring the top revenue cycle management trends shaping 2026, our market research team identified the following dominant themes:
- Automation across billing and coding workflows
- Widespread adoption of AI and machine learning
- Rising emphasis on value based reimbursement models
- Greater reliance on analytics driven revenue insights
- Enhanced patient financial engagement tools
- Constantly evolving regulatory and compliance demands
Drawing from these insights, this article highlights the top medical billing and RCM companies that are embracing these trends more effectively than others.
Best Revenue Cycle Management: Looking at it Side by Side
| Features | OmniMD | Athenahealth | Drchrono | Curemd | Advancedmd | Waystar | Tebra |
| Automated Denial & Appeal Management | ✔️ | Partial | ❌ | ✔️ | ✔️ | ✔️ | Partial |
| Specialty-Specific RCM Workflows | ✔️ | ✔️ | Partial | ✔️ | ✔️ | ❌ | Partial |
| AI-Driven Revenue & Financial Insights | ✔️ | Partial | ❌ | Partial | ✔️ | ✔️ | Partial |
| Integrated Patient Payment Automation | ✔️ | ✔️ | ✔️ | ✔️ | ✔️ | ✔️ | ✔️ |
| Full EHR + RCM Platform Integration | ✔️ | ✔️ | ✔️ | ✔️ | ✔️ | ❌ | ✔️ |
1. athenahealth
Founded in 1997, athenahealth transitioned from brick and mortar healthcare delivery to cloud based health IT, setting the stage for athenaCollector, its flagship revenue cycle platform.
Key RCM Capabilities
- Automated claim creation and submission
- Real time insurance eligibility checks
- Built in clearinghouse connectivity
- Integrated patient payment tools
- Regulatory compliance automation
- Advanced revenue analytics
Pros
- Strong payer connectivity
- Robust reporting tools
- Unified EHR and RCM ecosystem
Cons
- Higher pricing for smaller practices
- Limited customization for niche workflows
2. Drchrono
Established in 2009, Drchrono focuses on simplifying practice operations for small to mid sized clinics through a unified EHR, PMS, and billing suite.
Key RCM Capabilities
- Real time EHR to billing synchronization
- Mobile first billing access
- AI assisted coding suggestions
- Automated insurance verification
- Custom financial reporting
Pros
- Intuitive mobile experience
- Rapid deployment
- Ideal for independent practices
Cons
- Limited scalability for large enterprises
- Advanced analytics require upgrades
3. Curemd
Founded in 1997, Curemd blends cloud technology with consulting services, offering tailored RCM solutions supported by population health insights.
Key RCM Capabilities
- Waterfall billing automation
- Secondary payer management
- AI assisted code prediction
- End to end denial tracking
- Predictive cash flow modeling
Pros
- Highly configurable workflows
- Strong specialty customization
- Robust compliance safeguards
Cons
- Steeper learning curve
- UI may feel complex for new users
4. Advancedmd
Originally launched as Perfect Practice.MD, Advancedmd serves ambulatory practices with a scalable, cloud native revenue cycle platform.
Key RCM Capabilities
- Remote practice enablement
- Specialty specific billing logic
- Open database reporting
- Robotic process automation
- Flexible EHR integrations
Pros
- Highly extensible architecture
- Strong enterprise reporting
- Supports complex specialties
Cons
- Setup can be time intensive
- Requires configuration expertise
5. OmniMD
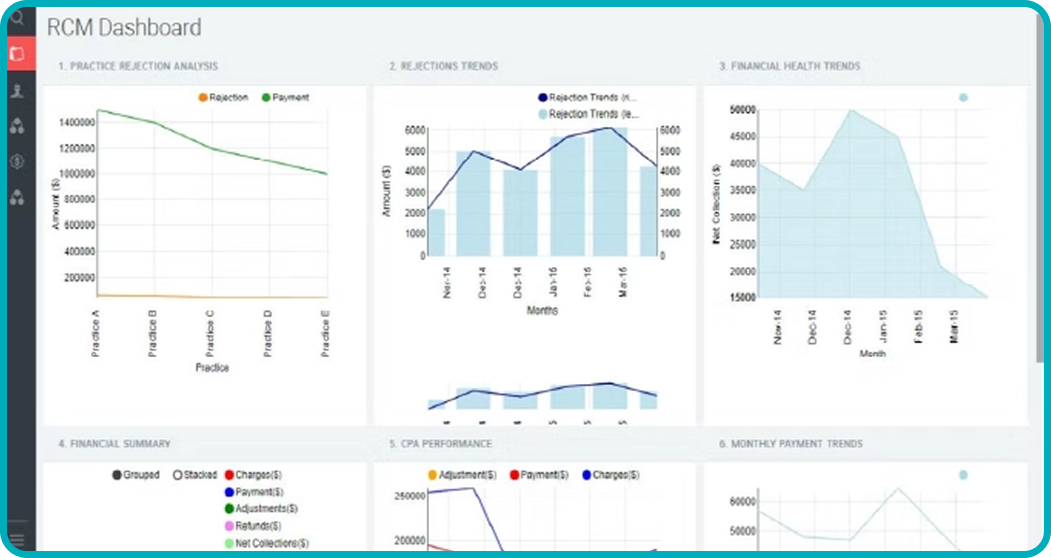
With more than two decades in healthcare technology, OmniMD delivers a unified, data driven RCM ecosystem designed to optimize profitability while ensuring seamless interoperability.
Key RCM Capabilities
- Specialty focused billing intelligence
- Predictive denial prevention
- Unified EHR and RCM architecture
- Automated eligibility and authorizations
- Advanced financial benchmarking
- Intelligent patient payment automation
Pros
- End to end platform consolidation
- Strong AI driven insights
- Enterprise grade compliance and security
Cons
- Best suited for organizations seeking full suite solutions
- Advanced features require onboarding alignment
6. Waystar
Waystar is a cloud based healthcare payments and RCM platform known for simplifying claim submission and reimbursement workflows.
Key RCM Capabilities
- Smart claim editing
- Automated denial detection
- Real time payer connectivity
- Integrated patient payment solutions
Pros
- User friendly interface
- Strong clearinghouse functionality
- Fast claims processing
Cons
- Limited native EHR features
- Custom reporting options are basic
7. tebra
tebra formerly known as kareo, primarily serves small practices with an emphasis on billing simplicity and rapid onboarding.
Key RCM Capabilities
- Simplified charge capture
- Built in patient statements
- Eligibility verification
- Revenue performance reporting
Pros
- Affordable pricing
- Easy implementation
- Strong customer support
Cons
- Limited automation depth
- Not ideal for high volume practices
Final Takeaway: Why Choose OmniMD
OmniMD stands as a paragon of modern revenue cycle management, seamlessly integrating EHR and RCM functionalities with AI driven intelligence. Its specialty focused workflows, predictive analytics, and real time financial insights empower healthcare providers to maximize revenue, streamline operations, and elevate patient engagement. With robust compliance safeguards and sophisticated automation, OmniMD offers a future ready platform that positions practices for sustained operational excellence in 2026 and beyond.
Frequently Asked Questions
Q: How does AI enhance medical billing efficiency?
AI elevates billing operations by automating coding, predicting and preventing claim denials, detecting anomalies, and optimizing workflows—ensuring accuracy, compliance, and operational agility.
Q: What advantages do cloud-based RCM solutions provide?
Cloud platforms deliver scalable, secure, and accessible infrastructure, enabling remote operations, seamless integration, automatic regulatory updates, and reduced IT overhead.
Q: What should a healthcare provider look for when selecting a medical billing solution?
Choose a platform that ensures regulatory compliance, integrates effortlessly with existing systems, leverages AI for intelligent automation, provides flexible deployment options, offers intuitive interfaces, supports efficient payment processing, delivers actionable analytics, and includes robust, continuous support and training.
Which factors should guide the selection of a modern medical billing solution?
- Compliance & Security: HIPAA adherence, encrypted data, and audit ready workflows.
- Seamless Integration: Compatibility with existing EHRs and practice management systems.
- Automation & Intelligence: AI assisted coding, claims management, and financial forecasting.
- Operational Flexibility: Cloud based accessibility or on premise control.
- User Experience: Intuitive dashboards and streamlined interfaces.
- Payment Processing: Online payments, automated invoicing, and digital wallets.
- Analytics & Reporting: Predictive financial insights, KPIs, and custom dashboards.
- Support & Training: Comprehensive onboarding, continuous support, and resource availability.
Disclaimer
We’ve built this resource with healthcare professionals in mind, ensuring that it saves you time and offers clarity in your decision making process. However, the comparison is based on independent research conducted by our team, leveraging publicly available information and vendor provided resources. Features and pricing details may vary; we recommend reaching out to the respective vendors for the most accurate and up to date information.

Choose the Best RCM Software
Leading the way in efficient, seamless healthcare payments

 Written by Divan Dave
Written by Divan Dave