Medical Billing Services
Built for clinics that think beyond collections, our HIPAA-compliant medical billing services are a strategic infrastructure that decodes complexity, neutralizes revenue leakage, and elevates operational economics with surgical accuracy.
Precision Billing for Faster Reimbursements
Revenue Cycle Expert
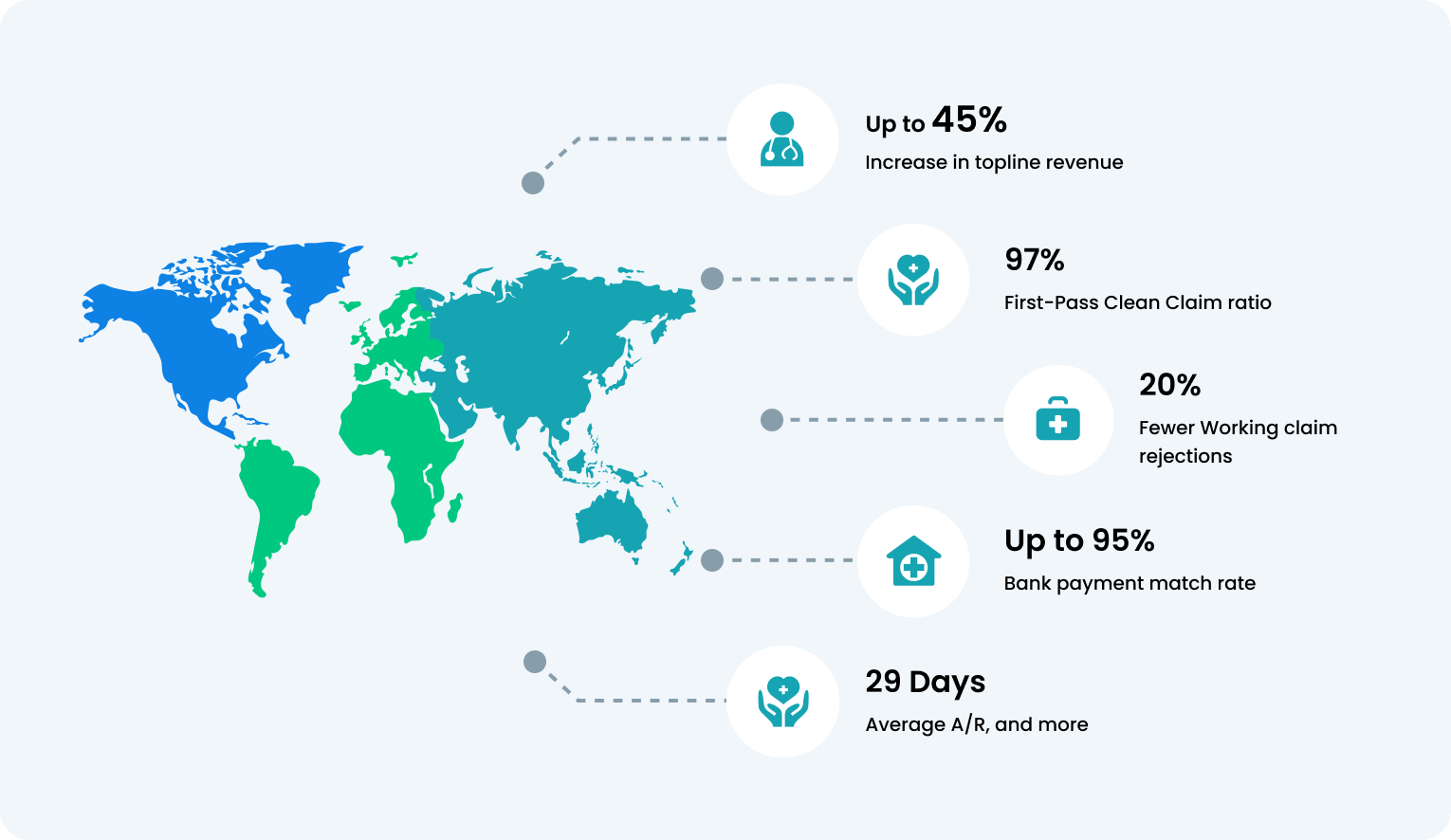
Our certified Revenue Cycle Experts use predictive analytics and payer behavior modeling to identify and eliminate inefficiencies in your billing lifecycle. With a proven track record of 97% first-pass clean claim ratio and accelerated cash conversion, your practice operates on financial autopilot, with no disruption to patient care or trust.

Dedicated Account Manager
Your Dedicated Account Manager becomes an extension of your team, monitoring revenue KPIs, handling payer escalations, and resolving claim issues with minimal effort from your side. Clinics report 94% satisfaction due to consistent communication, accountability, and proactive financial oversight.

Automated Claim Submission & Tracking
Experience faster claims, fewer errors, and full visibility with our medical billing services for clinics. Claims are auto-submitted through an advanced rules engine that adapts to each payer’s requirements, reducing rejections by up to 99.7%. Patients and staff can track billing status in real time through their portal, eliminating confusion and support calls.

Join 12,000+ Satisfied Healthcare Professionals
From solo providers to multisite groups, over 12000 clinicians trust our billing platforms to simplify their finances. In the first 90 days, most clients see fewer patient billing complaints, better portal transparency, and a measurable improvement in revenue predictability.

Advanced Reporting & Analysis
Our customizable dashboards go beyond basic reports. They highlight missed charges, payer delays, denial hotspots, and patient payment trends, all in plain language. Practices using our reporting tools typically see up to 20% increase in topline revenue without extra effort.

Certified Coding Support
We combine AI-assisted tools and certified coders to ensure every encounter is properly coded and compliant. This leads to a 39% drop in coding-related denials and helps maintain audit-readiness at all times, critical for avoiding payback requests.

Proactive A/R Follow-Up
Our A/R team uses smart prioritization and payer responsiveness scores to follow up on claims faster. On average, clinics cut 60+ day outstanding balances by 43%, improving patient portal satisfaction and stabilizing monthly revenue.

Denial Management
Every denial is traced to its source, be it coding, documentation, or front-desk workflows. Our tech and team work together to prevent repeat denials, with up to a 65% drop in denial recurrence seen within three billing cycles. Patients stay informed with automatic portal updates.


Best Medical Billing Services With
97% First-Pass Clean Claim Ratio
In a landscape where margins and time define survival, our outsourced medical billing services operates at the intersection of actuarial precision and clinical intelligence, achieving a verified 97% first-pass clean claim ratio.
Our team redesigns claim integrity at origin, embedding payer logic, compliance approach, and predictive edit layering before submission. Built for institutions that measure efficiency in certainty, not speed, our cloud-based medical billing services deliver financial continuity that is outcome-assured and architected for those who lead with foresight.
Round-the-Clock
Assistance
Uncompromising
Accuracy Standards
Analytics-Backed
Revenue Intelligence
State-of-the-Art
Solutions
Fast and Accurate
Payer Validation
Experience the OmniMD Advantage