Eliminate Denials and Rejections. Get paid faster & accurately.
Do you know 30% of your claims get rejected and/or denied?
Every practitioner knows claim rejections and denials can be tricky & complicated. That’s why it is critical that your claims are submitted clean the very first time. Claim denials can simply disrupt your cash flow. Efficient denial management is the key to effective revenue cycle management.
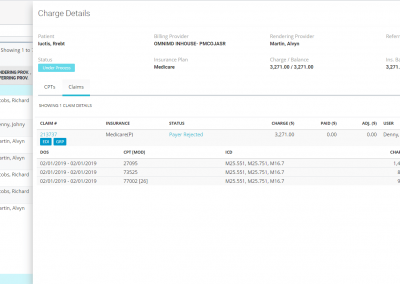
OmniMD RCM is a tool that provides details about every rejection and denial thereby allowing you to address the root cause of your denials and bring down the denial rate. Billers can easily broadly classify and flag denials that require review and efficiently resolve denials and resubmit insurance claims.
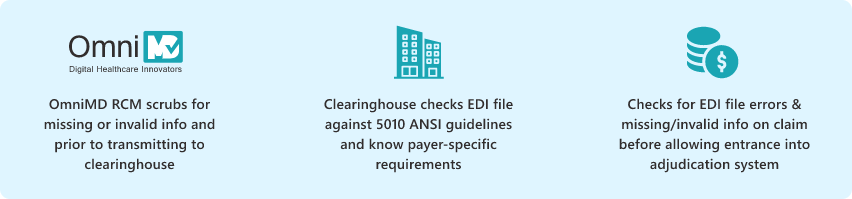
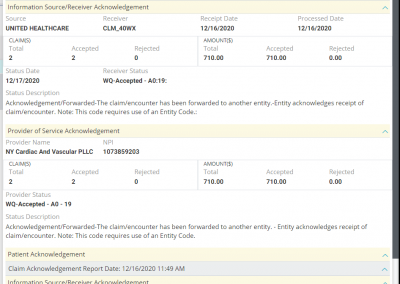
Before a claim is channelized into the payer adjudication system, the claim goes through a multistep validation process. With OmniMD RCM at each step, the rejected and denied claims are automatically categorized and put into separate buckets based on Clearinghouse and payer status reports, so you don’t have to necessarily login into the clearinghouse or payer portals to verify the status every time.
Each validation step reviews the claim for not only EDI file formatting rules but also for patient address, service location, CPT-ICD combination, payer ID, LCD and CCI guidelines, etc). If there is missing or invalid information, OmniMD RCM will sort those claims into scrub failed buckets and similarly any rejections and denials by clearinghouse or payer into respective buckets based on claim status and remark and rejection codes.
SUPPORTED EDI STANDARDS
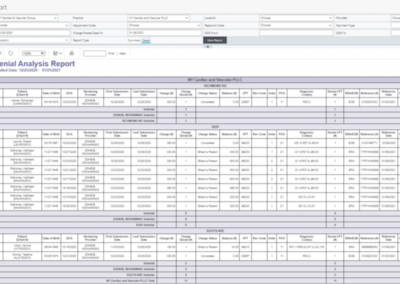
You can run detailed reports on CARC (Claim Adjustment Reason Codes) and RARC (Remittance Advice Remark Codes) to find the root cause of each denied claim and address the root cause. Preventing and reducing errors in your claims is the key to getting paid faster.
Clearinghouse Rejected and No Clearinghouse Response Claims
After you submit claims electronically, our integrated clearinghouse partners check the claims for any missing information and validate claims against payer-specific formatting requirements. You will receive a claim processing report that offers insight into Level 1 and Level 2 rejections, so you know exactly what needs to be fixed before submittal to payers. OmniMD provides hot links to such rejected claims for correction and resubmission.
Payer Rejected and No Payer Response Claims
After claims pass through the clearinghouse scrubbing engine, they are ought to be received by payers for adjudication and payment. At this point, these electronic claims pass through another set of validation against payer-specific requirements by the payer rule engine and are pushed back specifying the corrections before those claims can be accepted into the adjudication system. Also, at times these claims never reach the payer adjudication system. Based on time lag through the entire claim submission process, OmniMD provides hot links to classify such claims as ‘Payer Rejected’ and ‘No Payer Response.’
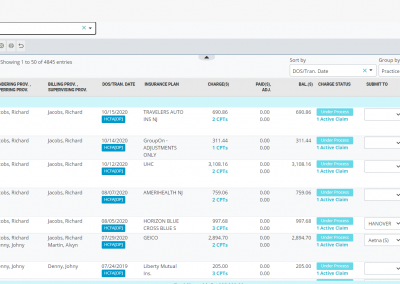
Accounts Receivable Manager (A/R Management)
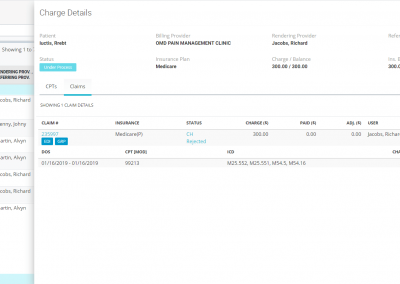
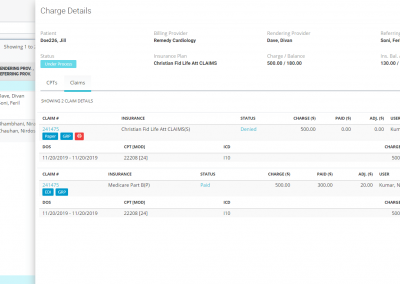
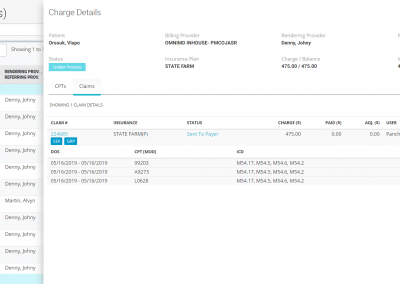
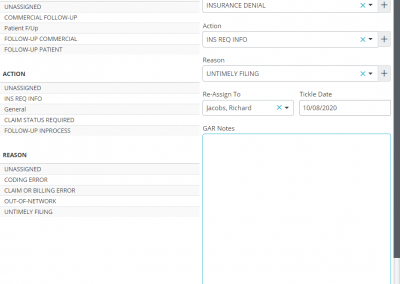
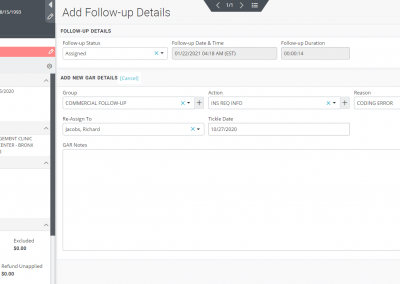
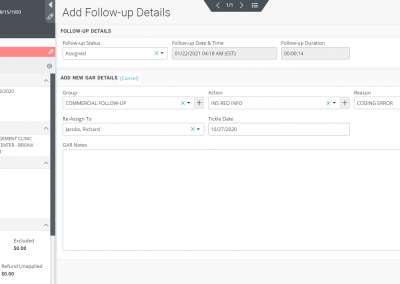
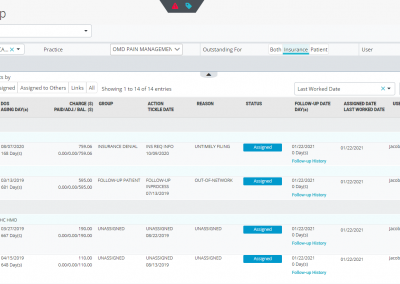
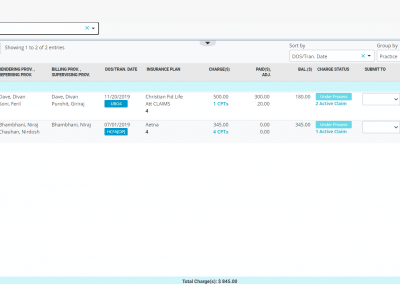
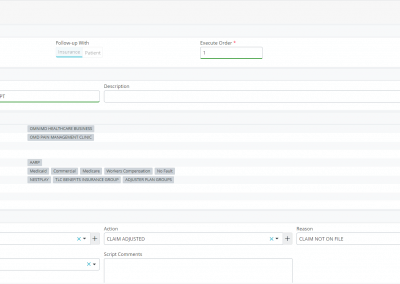
The claims segregated into rejection and denied buckets can further be categorized and organized into appropriate work queues. You can put each claim into what OmniMD RCM calls as “GAR” or “Group Action Reason” which helps you bunch these claims into either Medicare, Medicaid, or Commercial groups and define an action plan (e.g., claim resubmitted, appeal filed, medical notes requested, CLIA mapping required, send primary insurance EOB, etc.) and state a reason (example, bundled services, claim not on file, capitated, coding error, non-covered service, etc.) as to why such an action plan is required.
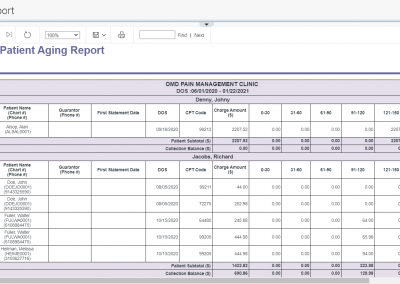
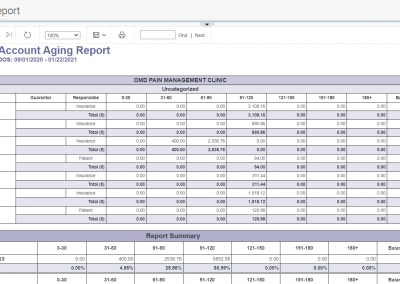
Aging Buckets-All vs Mine, Classification of Aging Tiers
Furthermore, you can classify your claims into folders named ‘high-value low aging,’ ‘high-value high aging,’ ‘low-value low aging,’ and ‘low-value high aging’ buckets and even link multiple service dates of same patient with common denial reason or multiple patients with common denials reasons for efficient and effective followup with the payers. The A/R manager provides a comprehensive snapshot of all information you need over the phone while addressing denials with the insurance company and also ability to capture notes and time these calls for better management of billing resources.
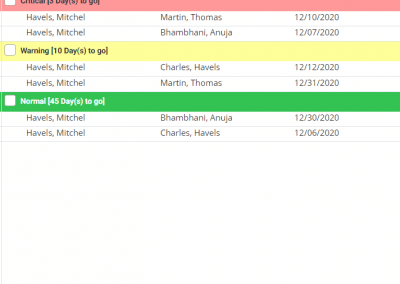
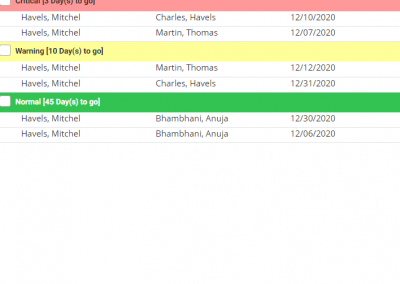
Timely Filing and Appeal Filing Notifications
OmniMD RCM software allows you to set custom to configure alerts and notifications based on payer timely filing and appeal filing deadlines – to pinpoint claims that may be stuck in the system. This helps you quickly recognize claims needing your immediate attention to be either corrected and resubmitted and/or send appeals to the payer, minimizing the number of unpaid claims.
Script Manager
Our far-reaching insurance follow-up module offers the ability to write scripts and execute them manually or in an automated way. With a script manager, you can not only automate your aging worklists but automate the allocation to your billers to bring on efficiency and effectiveness to your revenue cycle management process. A script filters claims to be followed up and moves claims into automated worklists as specified by GAR (Group/Action/Reason) for your billers automatically, e.g., the script on its own can filter out all Medicare claims that have not been followed up in 15 days (or time specified by you) and allocate all those claims to your dedicated billing staff working on Medicare only. No need for manual assignment of claims to be worked on to your billers. The script manager further allows you to write similar scripts to follow up on patient aging, not just insurance aging. You can write multiple scripts and even decide their execution order, both for insurance and patient aging dues.
Appeal and Collection Letters
Our integrated form designer allows you to incorporate and utilize standard appeal and collection letters as well as create custom appeal and collection letters that you can review, modify, print, or electronically fax from the system (with the date and time stamp for timely filing appeals).
Prevent denials with embedded and user-configured claim validation engine
Real-time claim submission status
Hot links to identify your lost claims
Hot links to identify your no response claims
Hot links to identify your rejected and denied/unpaid claims
Create transparent to-do lists allowing users to quickly identify claims needing attention
Track claim history
Script Manager to create automated work queues.
Robust reporting to provide insight into your rejections and denials to proactively respond and prevent future denials.
Billing Dashboard showing payer denial trends
Billing Dashboard showing payment velocity