Accurate Payment Posting is a key step and integral part of the medical billing cycle and provides a deep insight into the practice’s financial health and revenue stream and helps promptly catch potential fallouts and address them. A well-oiled payment processing tool and process help you identify payment trends, profit margins, opportunities to increase revenues, address denials faster, and iron out the deficiencies in the overall billing process.
An average of greater than 20% of medical payments are keyboarded manually due to the lack of the payer’s ability to provide a piece of electronic remittance advice (EDI 835 or ERA) back to the providers. This eventually costs a lot of time and resources to enter those payments manually. Furthermore, a wrong posting can result in inaccurate accounting causing unforeseen problems. ERAs and EFTs are advanced electronic tools allowing you to help save time and money.
OmniMD Medical Billing Software offers robust payment posting and processing tool to automate your payment posting process
Easy and quick EOB and ERAs reconciliation
Seamless credit card payment processing
Manage refunds and reversals with ease
Clear Patient responsibility
Segregating Denials faster
Faster remits with EFT deposits to your bank account.
Uncover underpayments and overpayments with contract management reports
Line items reporting containing payment details, non-covered services, refunds, and reversals.
Automated and quick Write-offs and adjustments
FEATURES
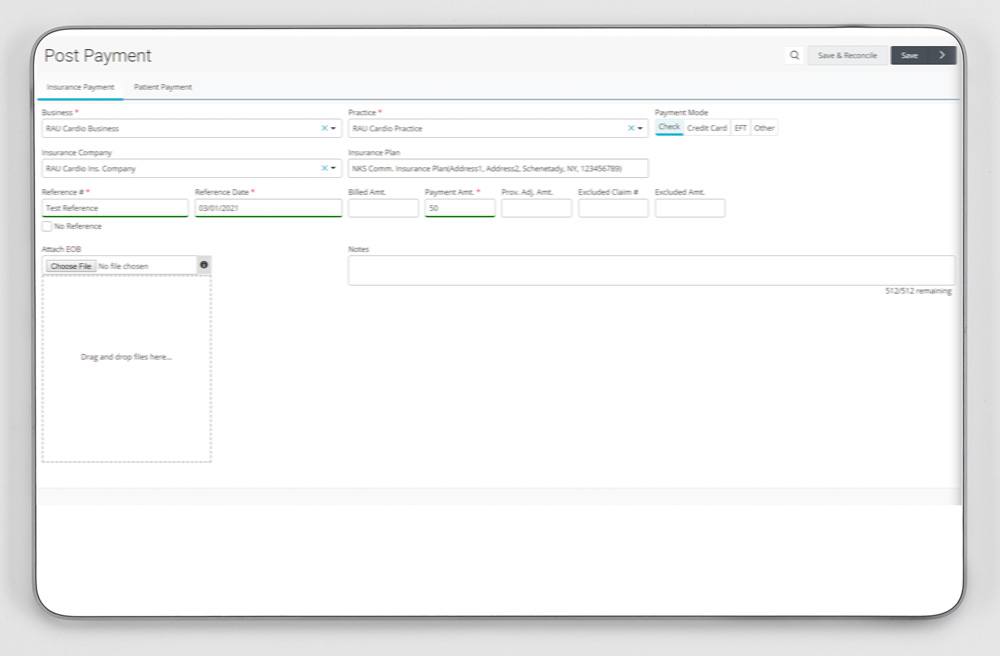
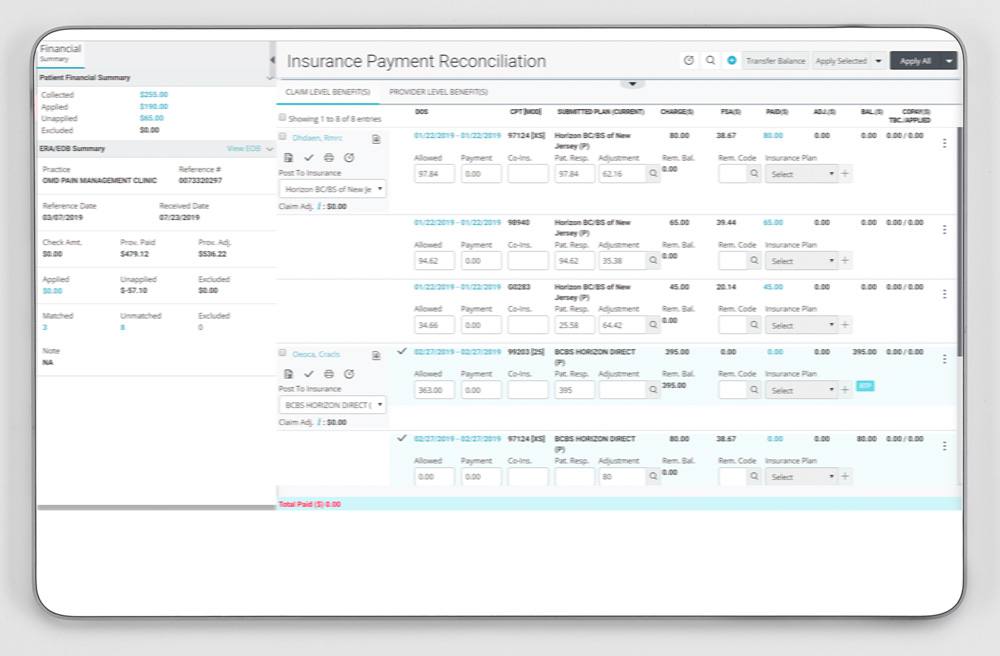
Accurate and Flexible Payment Posting
- Reconcile payments to the last penny accurately
- Quickly post payments for multiple responsible parties
- Post a single payment to all patients listed under one responsible party
- Accurate primary payment posting leads to accurate secondary payer billing
ERA Posting
- Convert most of your payers to electronic remittance
- Replace your process to post EOB manually and manually match payments
- Automated ERAs help you post hundreds of patients with one click
- A printable version of ERA makes it easier to submit COB (coordination of benefits) claims
- Eliminate manual posting to bring annual savings upwards of $10,000
- Easy denial organization
- Real-time analytical reports to provide better clarity on payment patterns and frequency
- Enhanced and focused collection efforts with electronic payment posting
- Address denials faster and decrease denials
EOB Posting
- Go paperless by scanning or dragging/dropping your scanned payments and denials
- Reconcile against a single or multiple responsible parties
- Reconcile a payment to all patients under one responsible party
- Avoid lost paper copies of payments and denials
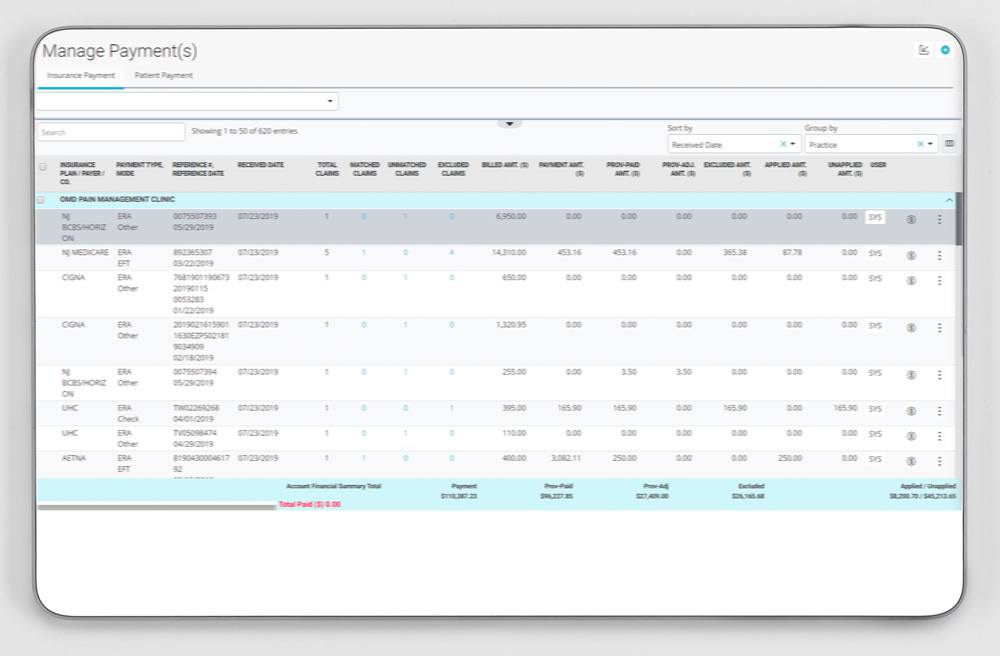
Electronic Funds Transfer (EFT)
- The secure, efficient, and convenient process to electronically deposit claim payments to bank accounts.
- Faster access to payments as compared to paper checks
- Easily match payments to remittances
- Secure and confidential deposits of claims payments
- Reduced handling time by staff members and paper usage, reducing administrative cost
- Easy to search and reporting tool
- Eliminate lost paper checks, inaccurate credit deposits, etc.
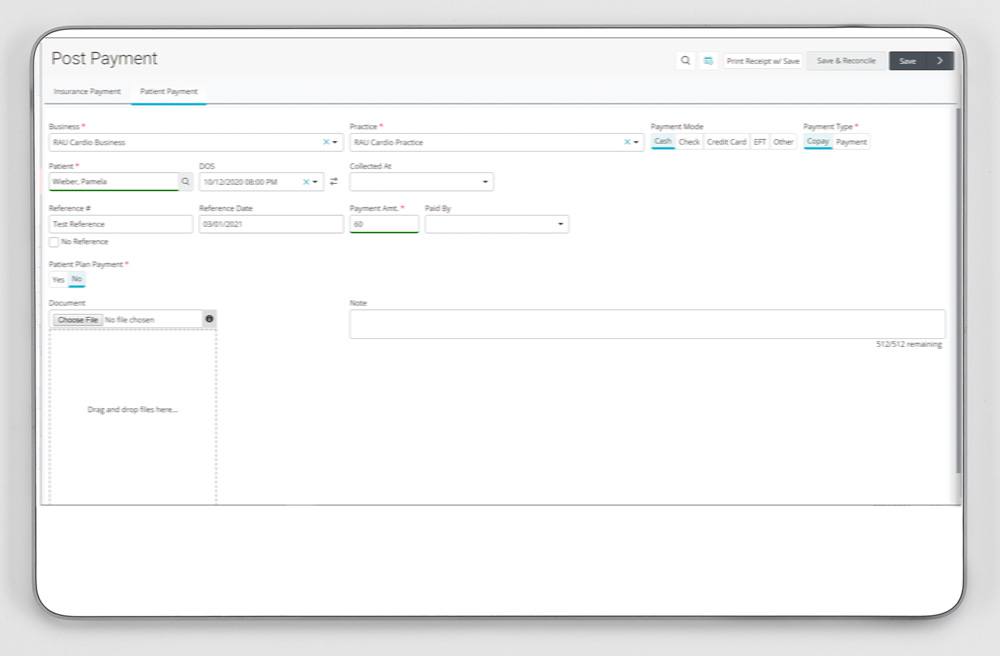
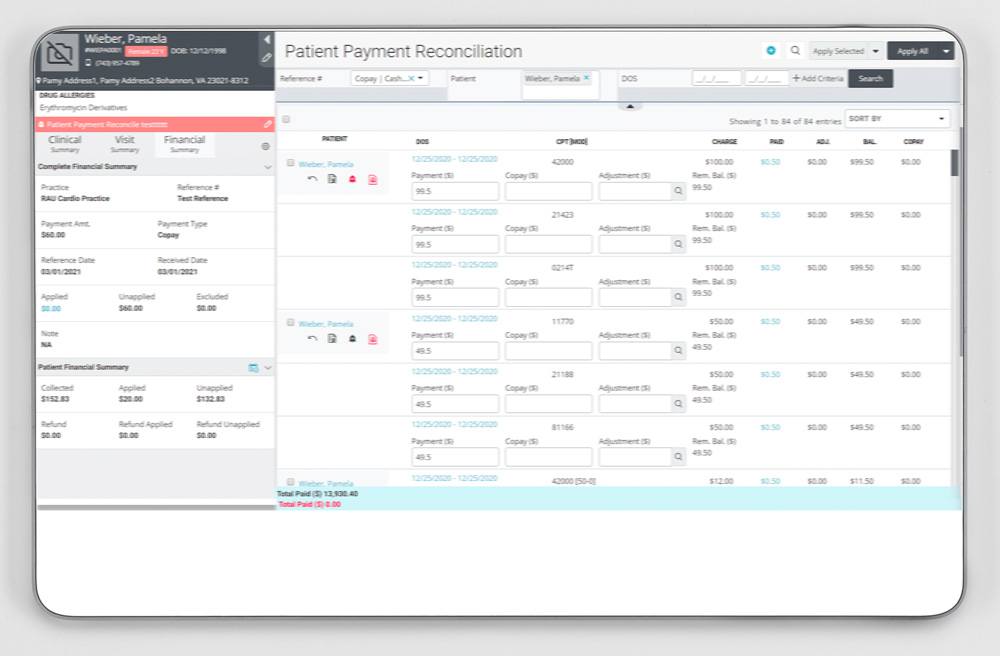
Increase Payment Collections with Credit Card Integration
- Accept patient payments seamlessly over the phone or at the office
- Accept payments via debit and credit cards
- Auto post credit card payments in your EHR or PM system
- Encryption of all financial transactions
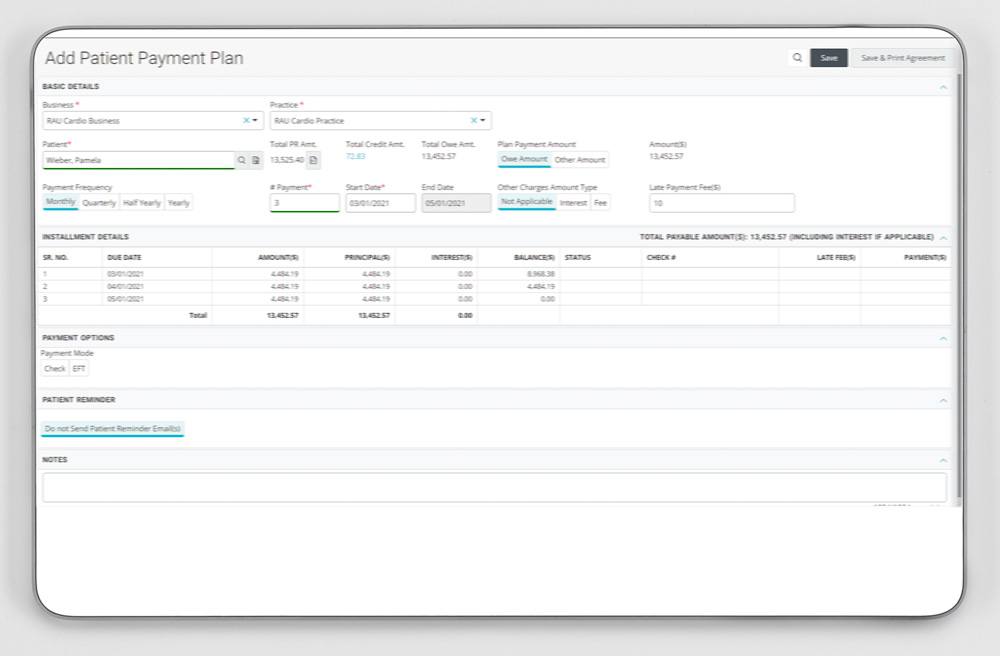
Flexible Payment Plan
- Create payment plan for your patients falling behind on payments
- Preview statements before processing