Medical Billing Software for Private Practices
Our HIPAA-compliant billing software redefines revenue cycle management by aligning clinical activity with real-time financial insights. Beyond automation, it delivers measurable gains in reimbursements, denial trend understanding, and payer behavior forecasting.
Redefining Medical Billing Software Excellence
Accounts Receivable
A focused, time-bound initiative to recover aging receivables and accelerate medical AR recovery. We segment and prioritize portfolios, apply proven AR follow-up workflows, and align with write-off governance to improve cash flow, reduce days in AR, close legacy balances, and strengthen financial hygiene across the healthcare revenue cycle.

Staffing Backfill
Rapid deployment of skilled revenue cycle management staffing and certified medical billing talent to stabilize operations during workforce gaps. Our resources integrate seamlessly into your existing RCM workflows, sustaining productivity and minimizing disruption across billing, coding, and AR functions.

Analytics & Insights
A comprehensive RCM analytics and reporting layer that turns raw data into actionable intelligence. We track core revenue cycle KPIs, AR Days, Denial Rate, Net Collection Rate, Clean Claim Rate, and DNFB (Discharged, Not Final Billed), enabling smarter decisions that improve cash flow, operational efficiency, and financial performance.

Medical Billing Software for Small Clinics
A fully integrated and accountable end-to-end medical billing solution for small practices. We manage registration through final payment using standardized RCM processes, automation tools, and compliance-first workflows. Our outcomes focus on cash acceleration, denial prevention, clean claim submission, and sustainable collection efficiency, purpose-built for small medical practices.
Financial Clearance Services
Pre-service rigor powered by automated insurance eligibility verification, benefits confirmation, prior authorization management, and accurate patient cost estimates. This front-end financial clearance model reduces downstream denials, enhances patient financial transparency, and maximizes point-of-service collections.
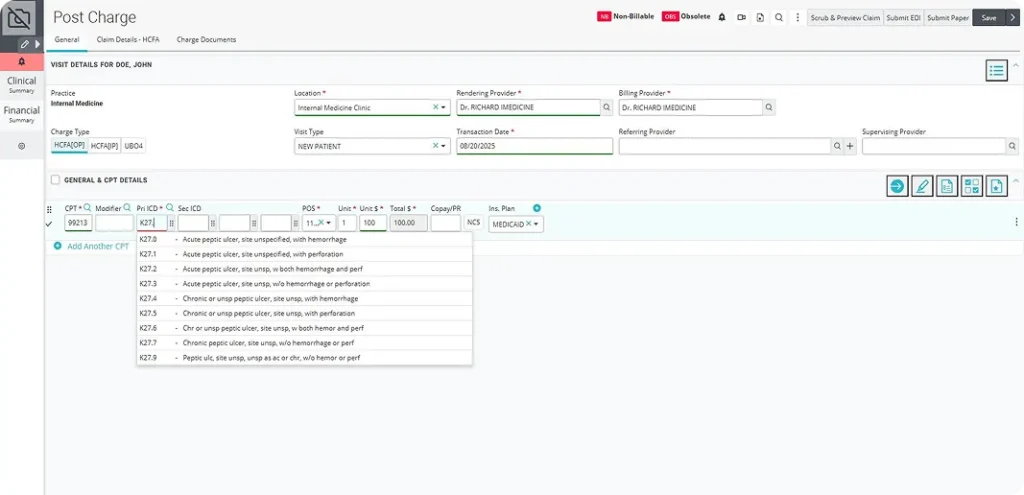
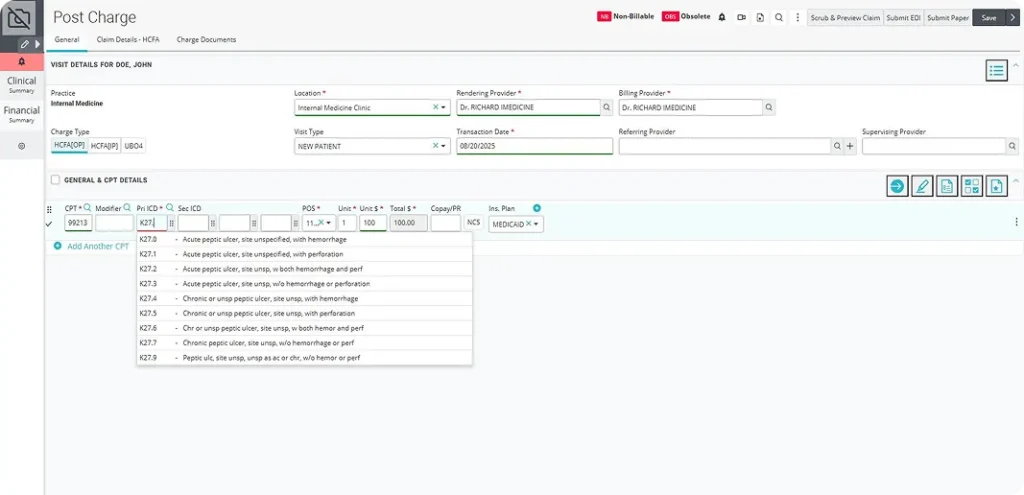
Coding Support Services
Certified medical coders and robust QA protocols ensure compliant medical coding services, accurate clinical abstraction, and payer-compliant documentation. We strengthen audit readiness, reduce coding-related denials, support HCC, E/M, CPT, ICD-10 accuracy, and optimize reimbursement integrity.

Accounts Receivable Follow-Up
Strategic AR follow-up services customized by payer patterns and account age. Our targeted workflows improve aging metrics, increase recovery, and reinforce upstream documentation and claim submission practices, reducing rework and preventing recurring AR issues.

Denials Management
A proactive denial prevention and resolution framework that addresses root causes, strengthens clean claim submission, and accelerates appeals. We reduce denial rates, improve overturn ratios, and implement denial management automation and corrective controls that prevent recurrence, ensuring faster reimbursement and predictable revenue.


Get 97% Claim Accuracy with Cloud-Based Medical Billing Software
Gain line-level clarity, predictive denials intelligence, and optimized work queues that prioritize action by impact with our cloud-based RCM software that delivers consistently high clean claim rates without compromising cycle speed or compliance. By unifying payer rules, charge integrity checks, and clinical documentation alignment into one adaptive ecosystem, it eliminates fragmented workflows that lead to denials.
Embedded AI continuously learns from remittance trends and payer behavior to fix revenue leakage. The system dynamically tunes edits and scrubbing protocols based on specialty, locality, and regulatory shifts with no manual rule-setting needed.